|
|
||||||||||||||||||||||||||||||||||
|
About Self-monitoring of blood glucose (SMBG)
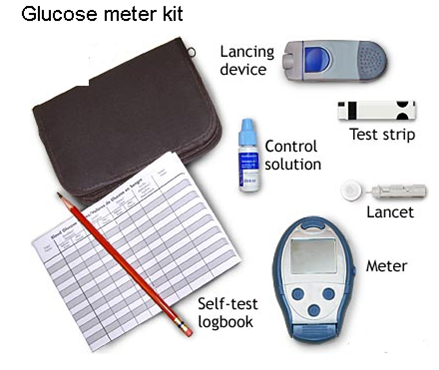
Self-monitoring of blood glucose (SMBG) with home blood glucose monitors is essential. The blood glucose (BG) results are used to assess the efficacy of therapy, and to provide data by which to make management decisions. Typically, patients who use insulin should check and record glucose levels at least 3-4 times per day. Some type 1's check as much as 6-8 times per day. Individuals with type 2 diabetes should be monitoring glucose levels, but if well controlled they may need somewhat less frequent checks. Patients on diet therapy without medications may only need to check BG a few times per week. Type 2's using oral agents should check at least 1-2 times daily, and vary the times. When BG control is sub-optimal, frequency of monitoring should be increased to provide data for therapy changes. To assure proper technique, patients should receive training on meter use. Blood sugar monitoring provides information about how the diabetes is doing. Don’t refer to the numbers as “good” or “bad.” The fact that the blood sugar is checked is good, no matter what the results are. Refer to numbers as "in target", or "out of target". If the number is above target, one can choose to do something about it. I can’t tell you how many people have come to their clinic appointments and have made up numbers to write in their logbooks. They didn’t want to write the high numbers down, so they made up numbers that they thought were better. Kids do it because they want to please their parents. Adolescents do it because sometimes they forget to test or don’t want to test as often as they are told to. I’ve even seen parents make up numbers in their child’s logbook because they were afraid the medical team would judge them for not being able to better control their child’s diabetes. I’ve seen pregnant women make up numbers to fool the team because they didn’t want to go on insulin. Some adults have done it because they didn’t know how to work the monitor and were too embarrassed to ask for help. There is no shame in having diabetes. Truthful, accurate blood sugar logs are critical in making decisions regarding treatment. It is so easy for the individual with diabetes to identify themselves with their numbers, and feel bad about themselves when the blood glucose isn't in control. We all need to treat the data non-judgmentally. Why Monitor the Blood Sugar? Blood glucose levels change throughout the day in relation to meals, medications, and activity. Stress, pain, and illness can also cause blood glucose fluctuations. Checking the blood glucose at various times of the day can provide a snapshot view of what’s happening. Assuring that the blood glucose is well controlled is critical in preventing diabetes-related complications. It is essential to use a glucose monitor because contrary to what many people think, one cannot really tell by feel the level of blood glucose unless it is extremely high or low. In order to avoid the microvascular complications of Diabetes we need to keep Pre-Meal glucose values below 7. We correlate the glucose monitoring result alongside the blood test called Hemoglobin A1c, glycated hemoglobin or A1c, this test measures the Average Glucose over a 3 month period. The hemoglobin A1c test provides important information and this test should be done every 3 months, but not in lieu of home blood glucose monitoring. Choosing a Meter There are many meters on the market. They are all pretty small and easy to use, some easier than others. Most meters have a memory and retain a record of blood glucose results. Some meters are downloadable and can provide computer printouts and graphs. Other meters have data management systems that allow input of data such as meal carbohydrate grams eaten, exercise, or insulin doses received. Meters are available for the visually impaired. A clear, step-by-step voice prompts the visually impaired person through the testing procedure. The technology is impressive. Cost of each test is about $1.00 (Cdn). What does a glucose-meter and monitoring supplies look like?
When to test The optimal time and frequency of SMBG depends on the patient's age, type of diabetes, type and timing of medication, co-morbidities, treatment goals, and history of glycemic control. Possible times to check blood glucose:
Record Keeping No one wants to review a meter's memory, number by number, and try to make sense of the information. A written logbook offers the added benefit of organizing blood sugar readings into the various times of the day. It allows both the patient and the health-care team to see glycemic patterns. When a reproducible pattern is observed, a treatment plan can be instituted. I advise patients to call when they notice a pattern that indicates inadequate control. All too often patients check their blood glucose levels, write down the numbers (or not), without using the information to problem solve. Patients have to be taught what to do with the numbers, and when to contact their healthcare providers. On the flip side, we health care providers must look at the blood glucose logbooks and interact with our patients regarding the numbers. Nothing is more frustrating for patients than to keep records and then have the healthcare team ignore the data. I recommend the use of a glucose diary, in such a diary there are usually columns for breakfast, lunch, suppertime & bedtime, you should put your glucose numbers in these columns (don’t bother with writing the time, it only makes the book confusing. At the end of the page, work out the average glucose for each column, then if you have time, you can work out the average for each time slot since you last saw the doctor or since you changed your medication. Computer printouts from the downloaded meter data are helpful, but shouldn't replace keeping written records. If patients just download their meter information the day of their appointment, then it's likely that they have not been reviewing the data on a daily and weekly basis, and are less likely to see patterns of control. |
||||||||||||||||||||||||||||||||||